**We are now performing Prostate Specific Membrane Antigen (PSMA) scans that target Prostate cancer, ask your Doctor if this is right for you or call for more information**
What is PET?
PET stands for Positron Emission Tomography. It is a procedure that adds an important dimension to our ability to diagnose and manage disease. Instead of detecting changes in the physical size or shape of internal organs (as with CT or MRI), PET detects changes in cellular function – how cells utilize nutrients like glucose. Since these functional changes often take place before anatomical changes occur, PET can provide information that enables your physician to make an earlier diagnosis. If abnormalities have already been detected by CT or MRI, PET can often better define the extent of disease, and characterize cellular function earlier in its course. This added information often means faster initiation of the best possible treatment, while avoiding more invasive exams or exploratory surgery.
“In all my years of being in and out of medical offices and hospitals, I have never been greeted or treated so kindly. The entire staff was pleasant and made me feel comfortable and at ease.”
How does PET work?
PET employs a positron-emitting radioisotope, Fluorine-18, coupled to glucose, a simple sugar; the resulting radiopharmaceutical is called fluorine-18 deoxyglucose, or FDG. Fluorine-18 is produced in a cyclotron and has an extremely short half-life (110 minutes), requiring that every dose be delivered to us within a few hours of when it will be used. Following intravenous injection, FDG is taken up by cells throughout the body, just as though it were glucose. Glucose is necessary for all metabolic activity in the body, and the cells that are most metabolically active take up more FDG than other cells. Once located inside cells, the distribution of FDG within the body can be imaged with a dedicated PET scanning system that incorporates a full ring of specialized detectors surrounding the body. At the time of its initial installation, River Radiology had the first and only dedicated PET scanner in the Mid-Hudson region (the GE “Advance” System).
What is PET-CT?
While PET scans alone are excellent for demonstrating areas of abnormal metabolism, the lack of anatomic features in the scans sometimes makes it difficult to pinpoint the exact location of a small abnormality seen within the patient. This is important, since FDG activity within a part of the intestine can be perfectly normal, but if the increased metabolic activity is actually located within a lymph node adjacent to the intestine, it may be abnormal. This problem has been solved by using sophisticated software to superimpose PET metabolic information directly onto a CT scan performed at the same time. This combined approach, called “PET-CT” or “Fusion” imaging, has been shown to increase the accuracy of PET scans by 20-30%.
When is it used?
A PET-CT study not only helps your physician diagnose a problem, it can also help predict the likely outcome of various treatment alternatives and monitor your progress. If you’re not responding as well as expected, you can be switched to a more effective therapy immediately. Today, PET is more and more frequently being used in the management of common cancers, including:
 |
|
Other uses of PET-CT include the evaluation of coronary artery disease and cognitive brain disorders. As additional positron-emitting radiopharmaceuticals are developed, it is expected that more uses for PET will be employed in the future.
Your PET-CT exam
This exam requires patient preparation in advance, including no solid foods for 6 hours prior to the exam, no strenuous activity for 3 days prior, and your last meal should be high in protein, low in carbohydrates. If you are diabetic, you must have a blood glucose level less than 200 mg/dl at the time of the examination, and you must not have taken insulin or other diabetic medication for four hours prior to your appointment. Wear metal-free clothing such as jogging or sweat pants with elastic waste and no zippers, and follow specific instructions if you are a diabetic patient. A nurse or technologist will administer an intravenous injection approximately 1 hour before the exam, after which you will relax in our “quiet room” while the injectable is absorbed throughout your body. It is important that you remain relaxed during the procedure. If you think you may require anti-anxiety medication, then you should bring it with you for your appointment, and take it when instructed by the technologist or nurse. Allow 2-1⁄2 hours for the appointment.
What should I bring to the appointment?
It is important that you hand carry your most recent X-ray/CT/MRI films to your appointment. The films can be returned to you before you leave, or we can mail them back for you.
What will happen during the PET-CT examination?
After receiving an intravenous injection of FDG, you will be asked to wait in a quiet room, without talking or moving, for 45-60 minutes. You will then be asked to lie on a comfortable table that moves slowly through the ring-like PET scanner. You should not feel a thing during the entire scanning procedure, which usually takes about 60 minutes to complete. You should plan on spending a total of 2-3 hours with us, from the time that you arrive until you’re ready to leave.
Are there any risks associated with PET-CT scanning?
PET is a very safe procedure. You will receive some radiation from the examination – roughly equivalent to what you might receive from X-rays or CT scans. Fluorine-18 has an extremely short physical and biological half-life, and quickly disappears from the body. Intravenous injection of FDG has not been reported to cause significant allergic reactions.
Are PET-CT scans covered by insurance?
PET is covered by Medicare and most other types of insurance, for the uses described above. Additional uses are being covered every year, so please ask your physician or call us for up-to-date information about insurance coverage.
When can my physician expect a copy of my report?
Most reports are available within a week and are accessible through our Patient Portal 4 business days after it has been read.
.
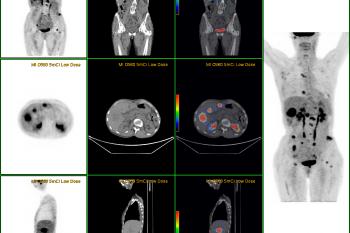
PET/CT FUSION of patient with history of COLON CA, mets seen in the mesentery.

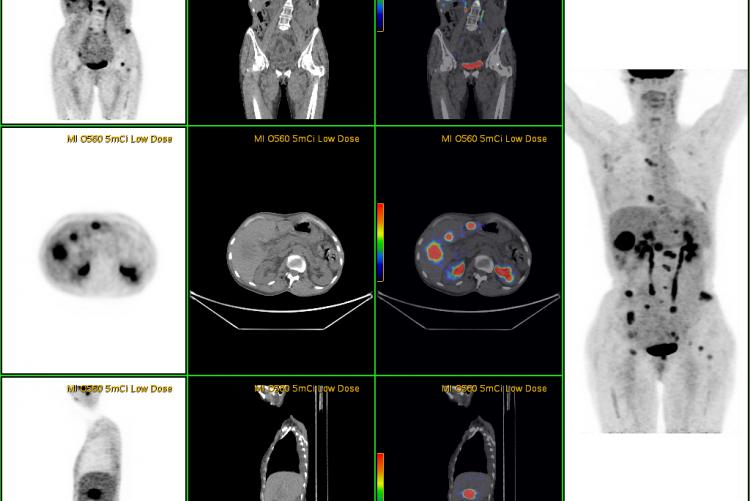
PET/CT FUSION performed on a patient with history of
ESOPHAGEAL CA, shows adrenal mets.

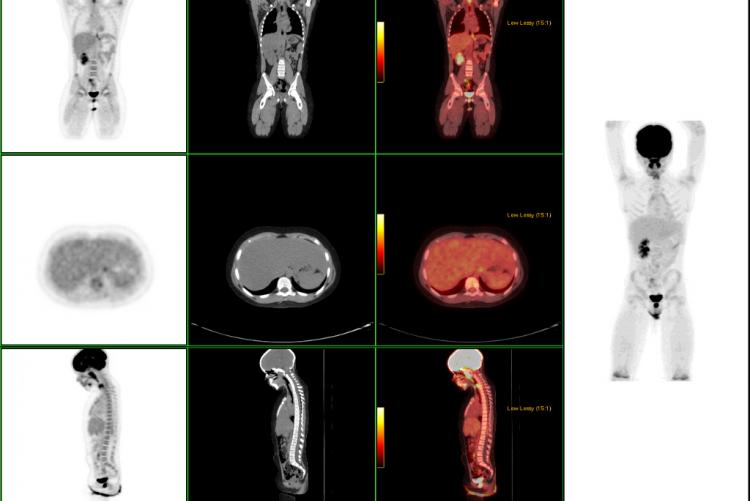
ESOPHAGEAL CA recently diagnosed, with no PET evidence that the cancer has spread to any other site.

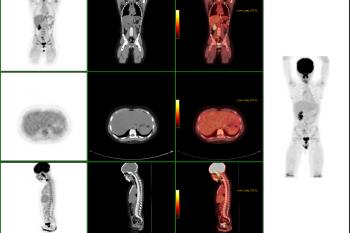
LUNG CA This patient has a history of breast cancer. Chest x-ray showed a spot on the left lung that could be pneumonia. PET showed the lungs to be a second primary site, not mets from the breast. There was no evidence that it had spread to the lymph nodes. CT has 65% accuracy, PET has 92% accuracy in staging lung cancer.

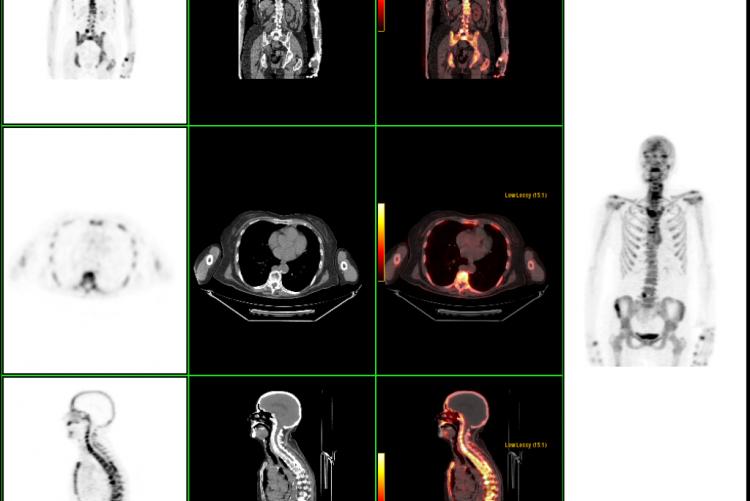
LYMPHOMA STAGING: Large chest mass with many small lymph nodes in the mediastinum and supraclavicular region. Nodes not appreciated on CT because they are normal in size. This proves to be stage 2 lymphoma because it involves 2 contiguous sites on one side of diaphragm.

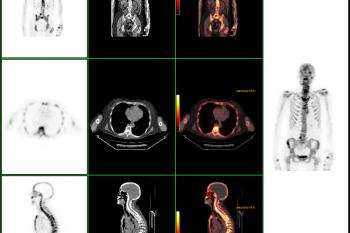
Coronal body section images from an actual PET scan. Increased tracer activity can be seen in the heart and urinary tract (which is normal) and also in a malignant lung tumor. There is no evidence that the lung tumor has spread to other parts of the body.